Significant Laboratory Test Charges for Controlled Substance Monitoring and Drugs of Abuse
Background
ClaimDOC’s comprehensive line-by-line auditing of claims uncovers errors that basic claim repricing and auto-adjudication does not catch, leading to greater savings for health plans and their plan members. Our audit team analyzes all types of healthcare claims for a variety of potential concerns including excessive usual and customary charges, duplication of claims, correct coding edits, unbundling of services, and many others. Our claims review is not intended to impact care decisions or medical practice.
In this Audit Spotlight, we focus on charges for laboratory services related to testing for controlled substance abuse monitoring and drugs of abuse.
Drug testing is used as a diagnostic and therapeutic tool for the clinical care and monitoring of an individual who is undergoing treatment for addiction.
Common drug testing may be presumptive or definitive. Presumptive drug testing also referred to as screening, involves qualitative analysis of a sample to determine whether a specific drug, drug metabolite, or substance is detectable above a threshold concentration. Definitive or confirmatory testing involves the analysis of a sample to determine how much (the quantity) of a drug or metabolite is present.
Medicare and numerous commercial health plans have medical coverage policies specific to laboratory drug tests. These medical policies outline benefits, coverage determinations, billing frequency parameters, coding and billing instructions, references, and other information.
What Accounts for Substantial Differences in Charges for Laboratory Drug Testing?
Charges for laboratory drug testing depend on the entity performing the test, the location where drug testing is performed, the specific CPT/HCPCS procedure code(s) reported/billed, actual drug testing costs, related markups for the drug tests, and other factors.
Case Example
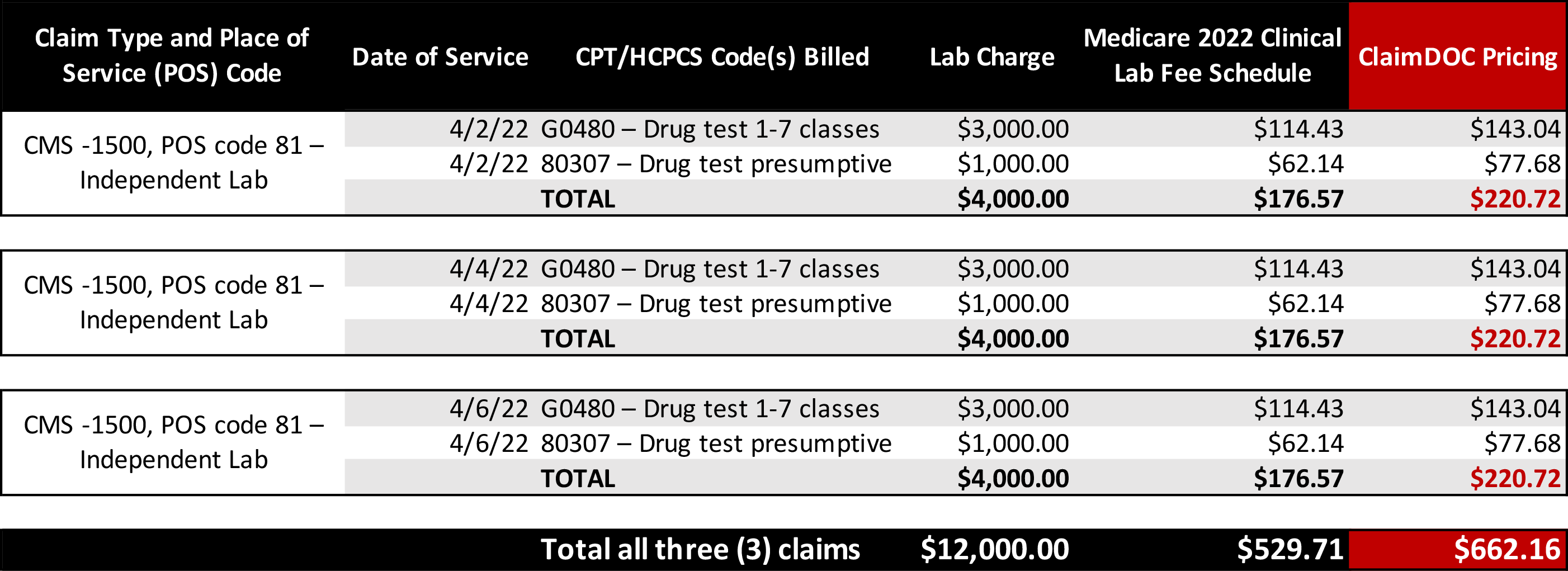
In the case example below, an independent laboratory located in Florida billed three separate claims for two (2) drug tests on three dates of service, April 2, 4, and 6, 2022 as follows:
*The Medicare Clinical Lab Fee Schedule (CLFS) payment amount for most tests equals the weighted median of private payor rates. CMS generally updates the CLFS private payor payment rates every 3 years and does not make geographic adjustments to the CLFS payment amounts.
Based on Medicare and other health plans’ medical coverage policies, presumptive/screening/qualitative drug testing is considered medically necessary when specific criteria are met. Billing frequency for drug testing varies among payors. For example, HPCPS code G0480 is not to exceed one (1) test per date of service up to sixteen tests a year. CPT code 80307 reported in the above example is not to exceed one (1) test per date of service up to thirty-two units per year. Another policy example limits testing not to exceed one (1) test per date of service, although there is no parameter related to how many total tests may be reported/billed in a year.
The Office of Inspector General (OIG) report dated June 2021, Opportunities Exist for CMS and Its Medicare Contractors to Strengthen Program Safeguards to Prevent and Detect Improper Payments for Drug Testing Services reflects, for calendar year (CY) 2019 (audit period), Medicare paid approximately $180 million for drug testing services provided to about 274,000 beneficiaries with substance use disorders nationwide. Although the overall Medicare fee-for-service improper payment rate was 7.3 percent for the Federal fiscal year 2019, the improper payment rate was 58.9 percent for the drug test with the highest Medicare fee schedule amount. OIG concluded with recommendations to CMS. CMS concurred with two of the five recommendations.
According to Market Intelligence Report, in 2019, national spending on mental health services totaled $225.1 billion and accounted for 5.5% of all health spending.
The Takeaway
Egregious charges were observed on the above independent laboratory claim. While laboratory providers may charge any amount they elect for any laboratory test, egregious fees can complicate matters for members to understand their bills and payments, impact the collection of patient balances, build a reputation of laboratories charging high fees, create burdens for patients having no insurance and a host of others.
Prices charged for laboratory drug tests vary widely within and across regions in the United States mainly due to traditional laboratory pricing power and consumers having been sheltered from costs due to insurance. With the implementation of the hospital price transparency mandate, effective January 1, 2021, accessible online pricing information makes it easier for consumers to shop and compare prices across hospitals and estimate the care costs.
Our goal at ClaimDOC is to use benchmark charges and costs nationally to negotiate fair and ethical payments. Employers turn to us to establish fair reimbursement rates for their plans allowing them to save money and provide richer benefits to their employees. A win-win for everyone.