Significant Variations in Charges for Routine Colonoscopy Services
Background
ClaimDOC’s comprehensive line-by-line review of claims uncovers errors that basic claim repricing and auto-adjudication does not catch, leading to greater savings for health plans and its plan members. Our audit team analyzes all types of healthcare claims for a variety of potential concerns, including excessive usual and customary charges, duplication of claims, incorrect coding, unbundling of services, and many others. Our claims review is not intended to impact care decisions or medical practice.
In this Claims Audit Spotlight, we focus on colonoscopy services and their related charges. Colonoscopy is the most commonly performed gastrointestinal procedure, with over 16 million colonoscopies in the United States each year. Colonoscopies are performed as a screening for cancer, surveillance, and diagnostic to evaluate symptoms.
How Much Does a Colonoscopy Cost?
Typical costs for colonoscopy services vary widely due to a variety of factors. Charges depend on several factors:
- Where the colonoscopy is performed, for example, in an ambulatory surgical center (ASC), hospital outpatient department, a physician’s office location or less seldom, in a hospital inpatient setting.
- The applicable CPT/HCPCS code(s), modifier(s), diagnosis code(s), and other information reported/billed on the claim.
- The type of insurance the patient has or no insurance/self-pay.
- Health insurance plan language and specific details related to “screening” and “diagnostic” tests/procedures.
Typically, there is a charge for the facility component and a charge for the professional component (practitioner performing the procedure). There may also be additional professional charges billed by a pathologist and/or an anesthesia practitioner and a cost for the preparation kit needed for the procedure.
Federal Law
The Affordable Care Act (ACA) requires both Medicare and private insurers to cover the costs of preventive colorectal cancer screening tests, as these tests are recommended by the United States Preventive Services Task Force (USPSTF). The law specifies that there should be no out-of-pocket costs for patients, such as co-pays or deductibles, for these screening tests.
Private Health Insurance Coverage for Colorectal Cancer Screening
The ACA requires health plans that started on or after September 23, 2010 to cover colorectal cancer screening tests, which includes a range of test options. In most cases, there should be no out-of-pocket costs (such as co-pays or deductibles) for these tests.
There are nuances related to colonoscopy coverage, as the definition of “screening” can oftentimes be confusing. Colonoscopies classified as “diagnostic” are not applicable under the provisions of the ACA. It is important providers, coders, and billing staff understand the proper reporting and billing of colonoscopy services. Some plan policies may not cover other costs associated with colonoscopy screening services and some may have certain costs for particular plan holders.
What Accounts for the Large Differences in Colonoscopy Charges?
As referenced above, charges for colonoscopy services depend on the specific ASC, hospital, practitioner, the locality/state where the colonoscopy is performed, and the applicable CPT/HCPCS procedure code(s) and information reported/billed on the claim.
Case Scenario
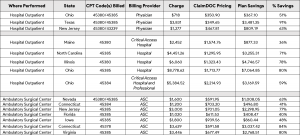
Outlined below are claim examples detailing where colonoscopy services are performed, CPT code(s) billed, billing provider, associated charge, ClaimDOC pricing, plan savings, and percent of savings.
Physician (Professional) and Facility Claims
The Takeaway
As referenced above, there are large differences in charges for colonoscopy services. Healthcare policies are complex, often making it difficult to understand the full extent of a member’s coverage and benefits. Prior to colonoscopy services being performed, consider options of where to have the procedure and obtain a fee estimate of the cost.
Inquiries/communications with health plans and providers can assist in determining the financial liability for preventive or diagnostic colonoscopy services. Ask questions related to applicable age limits, frequency parameters, coverage for pathology services, anesthesia services, if preparation kits are included in the plan if there are partnerships with selected providers to obtain discounts, and other issues/concerns. Being armed with information in advance of an elective procedure can help eliminate fears of “surprise” billing and unexpected costs.
Our goal at ClaimDOC is to use benchmark charges and costs nationally to negotiate fair and ethical payments. Employers turn to us to establish fair reimbursement rates for their plans allowing them to save money and provide richer benefits to their employees. A win-win for everyone.