What is a Reasonable Fee? Substantial Disparities Among Charges for CT Scans
Background
ClaimDOC’s comprehensive line-by-line review of claims uncovers errors that basic claim repricing and auto-adjudication does not catch, leading to greater savings for health plans and its plan members. Our audit team analyzes all types of healthcare claims for a variety of potential concerns including excessive usual and customary charges, duplication of claims, incorrect coding, unbundling of services and many others. Our claims review is not intended to impact care decisions or medical practice.
In this Audit Spotlight, we focus on members undergoing a diagnostic CT scan and the related charges reported and billed by various providers for imaging services. Each billing entity in our analysis reported/billed the diagnostic CT scan using CPT code 74176 (without modifier).
Increase in CT Scan Usage
According to a Harvard Health Publishing article dated, September 30, 2021, “over 80 million CT scans are performed in the United States each year, compared with just three million in 1980.”
Coding/Billing for CT Scan Services
Computed tomography is commonly referred to as a CT scan. A CT scan is a diagnostic imaging procedure that uses a combination of X-rays and computer technology to produce a cross-section of the body. It shows detailed images of selected part(s) of the body, including bones, muscles, fat, organs, and blood vessels. The scan may performed without a contrast agent (dye) or it may be performed with contrast. There are numerous CPT codes for the reporting and billing of CT scan services, depending on the area of the body being imaged, whether performed without contrast, with contrast or without contrast followed by contrast and further sections/sequences. Additionally, CT scans may be considered a global code (no modifier, encompassing both the technical component and professional component), a professional component only service (reported with modifier 26) or a technical component only service (reported with modifier TC).
Based on the practitioner order, the abdomen and pelvis frequently undergo CT imaging at the same time, for example to evaluate a patient following trauma or for conditions such as appendicitis, diverticulitis, ulcerative colitis, and cancer.
The following three CPT codes describe same-session CT imaging of the abdomen and pelvis:
- 74176, Computed tomography, abdomen and pelvis; without contrast material
- 74177, Computed tomography, abdomen and pelvis; with contrast material(s)
- 74178, Computed tomography, abdomen and pelvis; without contrast material in one or both body regions, followed by contrast material(s) and further sections in one or both body regions.
Claims Analysis and Disparities Indentified in Charges for CT Scan – CPT Code 74176
Factors that affect the charge for a CT scan can vary significantly depending on:
- The type of CT scan ordered by the practitioner
- The facility type where the CT scan is performed
- If uninsured or insured
- If the provider is in-network or out-of-network
- The location (city/state) where the imaging is performed
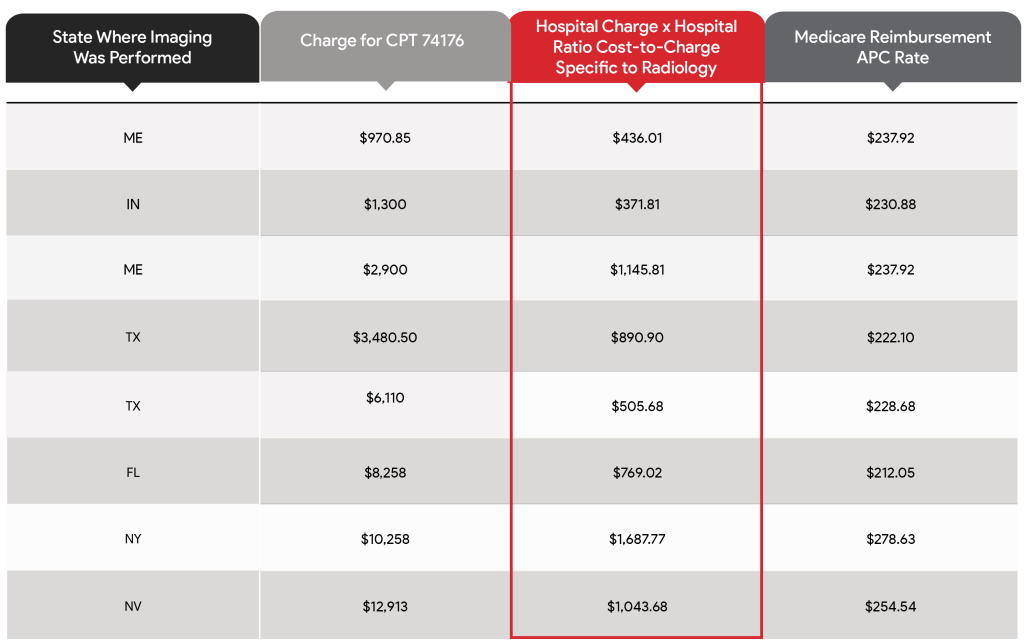
Examples of Hospital Outpatient Charges for CPT Code 74176 – CT Scan of Abdomen and Pelvis without Contrast Reported/Billed on UB-04 Claim Form/Electronic Equivalent – Services Provided in 2023
The Takeaway
Charges for the same CT scan varies greatly between facilities depending on the provider and where testing services are performed. Our analysis identified:
- Charges ranged from $970.85 to $12,913.00 when CT scan was performed in a hospital outpatient setting.
- During our analysis, we additionally identified an egregious charge of $21,524.75 when a CT scan (CPT code 74176) was performed in a hospital inpatient setting.
- Hospitals use their chargemaster, a list of procedure codes with corresponding prices for thousands of items/services, to record services provided, determine the charges for each service and generate hospital bills. Hospital rates are typically established by individual hospitals and with few exceptions, are not subject to charge limitations in most states. As noted above, the charges for services are often several times the Medicare-allowable cost of providing the designated service.
Imaging Procedure Checklist
- Regardless which diagnostic test the practitioner recommends/orders, when given the opportunity of selecting a provider of service, check if the procedure can be performed in an outpatient setting and the availability of a freestanding diagnostic imaging center(s) or clinic(s) offering CT services in your area.
- Search for the best value in your location and keep a record. If you receive a medical bill that is higher than expected, this information can be useful.
- Depending on the type of insurance, it is important to determine if the provider performing the procedure is in-network. Sometimes a provider who treats you is designated as being out-of-network. Inquire whether all of the providers who will treat you are in-network for your insurance.
ClaimDOC’s Comprehensive Claims Review and Goals
The improper reporting of services, coding/billing errors and egregious charges can complicate matters for members to understand their healthcare bills and payments, impact the collection of patient balances, build a reputation of providers charging high fees, create burdens for patients having no insurance and a host of others.
When an individual receives a bill for healthcare services appearing questionable/inappropriate, an inquiry to the provider and/or health plan should be made to obtain an explanation of the service(s), corresponding charges, and reimbursement.
Our goal at ClaimDOC is to use benchmark charges and costs nationally to negotiate fair and ethical payments. Our high-quality and expert review of claims identifies and prevents improper medical claim payments and maximizes long-term cost savings opportunities. Employers turn to us seeking to establish fair reimbursement rates for their plans allowing them to save money and provide richer benefits to their employees. A win-win for everyone.