Everything is Bigger in Texas – Including Physician Charges
Background
ClaimDOC’s comprehensive line-by-line auditing of claims uncovers errors that basic claim repricing and auto-adjudication does not catch, leading to greater savings for health plans and its plan members. Our audit team analyzes all types of healthcare claims for a variety of potential concerns, including excessive usual and customary charges, duplication of claims, correct coding edits, unbundling of services, and many others. Our claims review is not intended to impact care decisions or medical practice.
In this Claims Audit Spotlight, we focus on a physician claim example where our audit team reviewed the claim for the procedures reported/billed and the related physician charges. We raised the red flag and asked three (3) questions:
- Is there a mistake in physician billing on this claim?
- Is the physician really charging this much for the billed procedures?
- What are other physicians in the same or surrounding area charging for the same services?
Case Scenario
A 47-year-old male was seen at an ambulatory surgical center (ASC) in Texas for the treatment of neck pain. Based on the claim information, the procedures performed by the physician involved inserting a needle through the skin into the proper position within the cervical or thoracic facet joint(s), using CT imaging guidance or fluoroscopy. A single or a combination of techniques (i.e., thermal, electric, chemical, radiofrequency) is used to destroy the nerve root(s). The administration of intravenous medication was also billed.
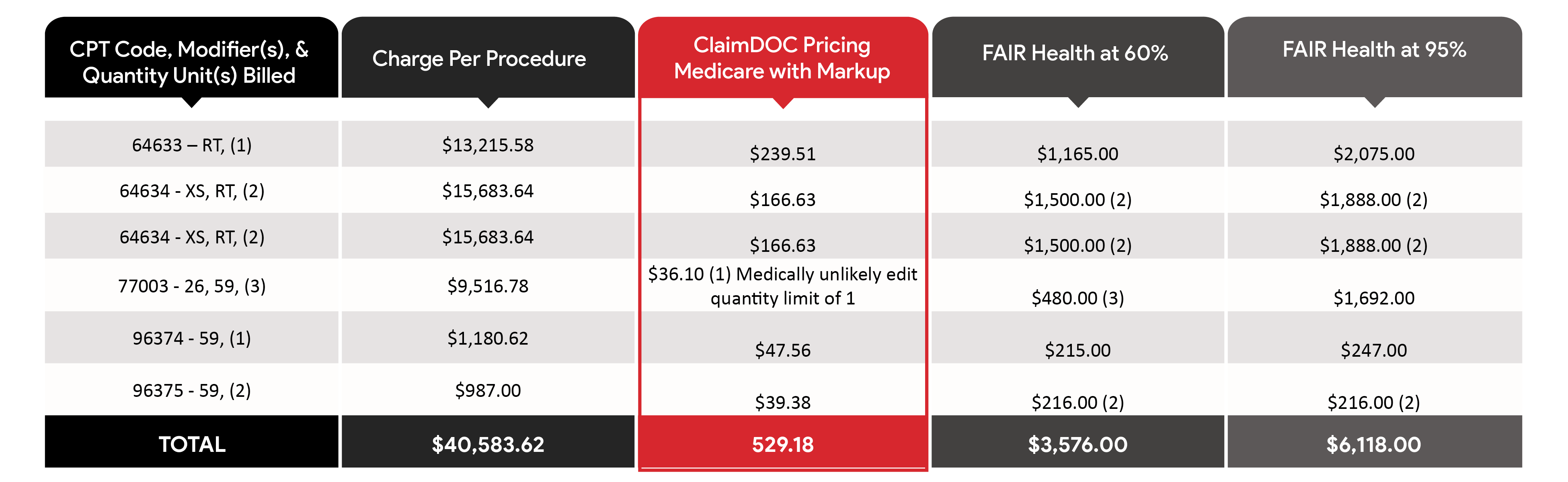
The physician reported/billed the following services on the CMS-1500 claim form/electronic equivalent. Additionally, information includes ClaimDOC’s pricing, plan savings, and FAIR Health physician charge data comparisons at the 60th and 95th percentiles for physician services charged/provided in the same or surrounding physician locality.
Total hospital charge – $40,583.62
ClaimDOC Pricing: $529.18
Plan Savings: $40,054.44
Percentage of Savings: 99%
The Takeaway
Egregious charges for the procedures billed were identified on the above physician’s health insurance claim. While physicians may charge any amount they choose for items/services provided with few exceptions, egregious fees, and billing errors can complicate matters for members to understand their bills and payments, impact the collection of patient balances, build a reputation of providers charging high fees, create burdens for patients having no insurance and a host of other issues.
Obtaining a price estimate prior to needing or having related medical care to understand how much an individual is obligated to pay for their services can be beneficial to avoid surprise medical bills. Whenever an individual receives a bill, and the cost for care seems inappropriate/questionable, an inquiry to the provider and/or health plan should be made to obtain an explanation of the service(s) and corresponding charges.
Our goal at ClaimDOC is to use benchmark charges and costs nationally to negotiate fair and ethical payments. Employers turn to us to establish fair reimbursement rates for their plans allowing them to save money and provide richer benefits to their employees. A win-win for everyone.